The COVID-19 pandemic has brought to light many health issues, some of which are still being studied. One such condition that has seen an alarming rise is Avascular Necrosis (AVN) of the hip joint, particularly in post-COVID patients. AVN, also known as osteonecrosis, is a serious and painful condition that can lead to the destruction of the hip joint if left untreated. This article explores AVN, its causes, its relation to COVID-19 and available treatments.
What is AVN?
Avascular Necrosis (AVN) occurs when the blood supply to the bone tissue is interrupted or reduced, leading to the death of bone cells. Over time, this can result in the collapse of the bone structure, particularly in weight-bearing joints such as the hip. When the hip joint is affected, patients experience severe pain, stiffness, and difficulty with movement.
Causes of AVN
There are several known causes of AVN, including:
Trauma: Injury to the hip joint, such as a fracture or dislocation, can damage blood vessels, leading to AVN.
Steroid Use: Long-term use of corticosteroids, which are often prescribed to reduce inflammation, has been linked to an increased risk of AVN.
Alcohol Abuse: Excessive alcohol intake can interfere with blood flow to the bones, raising the risk of AVN.
Medical Conditions: Conditions such as sickle cell anemia, lupus, and certain blood disorders can increase susceptibility to AVN.
Many patients who were treated with high doses of corticosteroids during severe COVID-19 cases have developed AVN, particularly in the hip joint.
SEE MORE: Stages of AVN
Increased Incidences of AVN Post-COVID
Recent studies have shown that post-COVID AVN cases have increased by 10 times compared to pre-pandemic levels. This spike is particularly concerning in young male patients, who are disproportionately affected. The male-to-female ratio in AVN cases stands at approximately 5:1, indicating that men are far more likely to develop this condition.
AVN can occur at any age, but the increased incidence in young adults is alarming because of its long-term implications on mobility and quality of life.
The condition’s rise necessitates early diagnosis and specialized treatment from an experienced orthopedic surgeon in Ahmedabad like Dr. Rachit Sheth at Synergy Hospital (Gota, Ahmedabad).
Medical Management of AVN
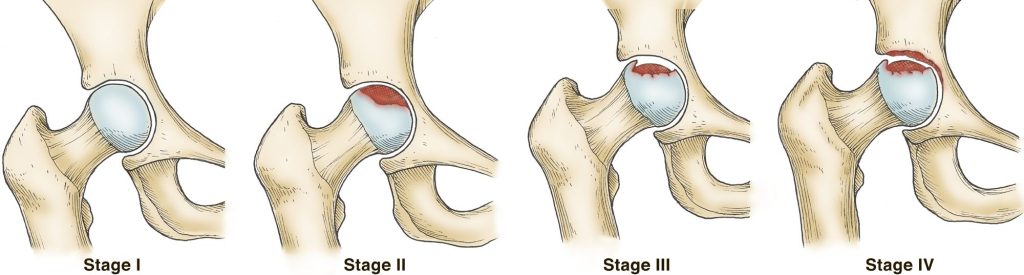
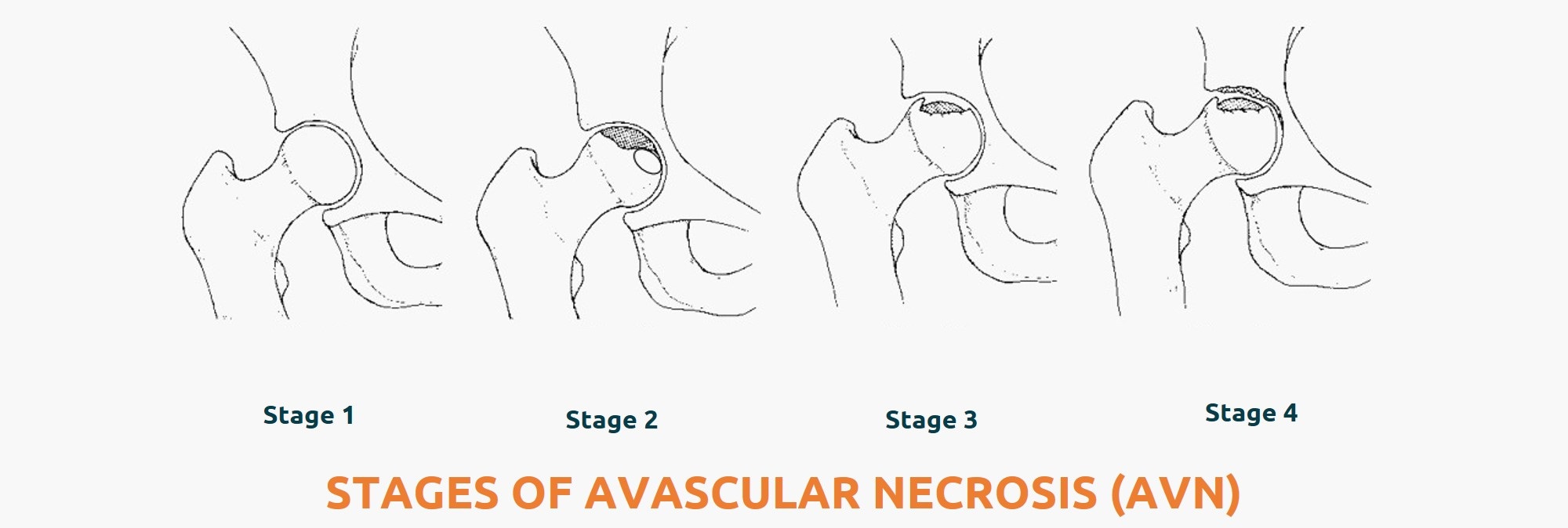
Early diagnosis is crucial for the effective management of AVN. The condition progresses through several stages, from mild pain in the early stages to complete joint collapse in advanced cases. Medical management is possible in the early stages (Stage 1 and 2-A). Treatment options include:
Medications: Bisphosphonates and anticoagulants may help slow the progression of bone damage and improve symptoms.
Physical Therapy: Strengthening the muscles around the hip can help alleviate symptoms and improve mobility.
Lifestyle Changes: Limiting alcohol consumption, stopping steroid use when possible, and addressing underlying health conditions are crucial for managing AVN.
However, AVN has a tendency to progress rapidly, especially without early intervention.
Core Decompression and Stem Cell Therapy (Up to Stage 2-A)
For patients diagnosed in the early stages of AVN, Core Decompression combined with Stem Cell Therapy/Platelet Rich Plasma Therapy has shown promising results. This minimally invasive surgical procedure involves removing a small portion of the bone to reduce pressure within the joint and promote new blood vessel formation. Stem cells are then introduced to stimulate bone regeneration and repair.
Core decompression is most effective in patients with Stage 1 or early Stage 2-A AVN. At these stages, the hip joint can often be preserved, delaying or preventing the need for more invasive procedures.
Total Hip Replacement (THR) for Advanced AVN
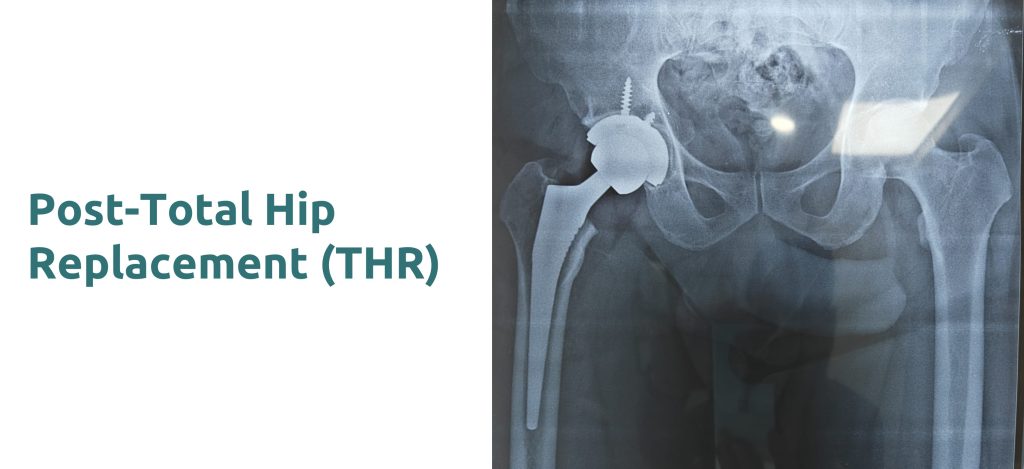
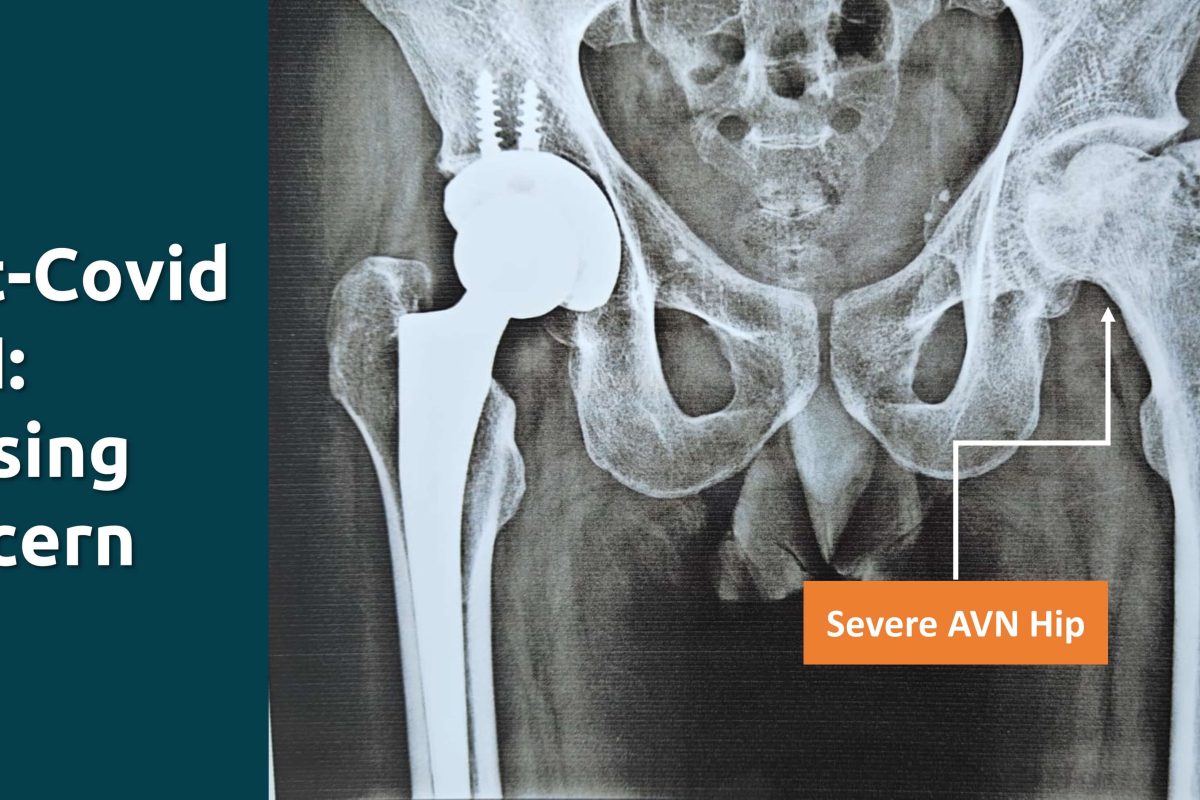
Once AVN progresses to Stage 3, the damage to the bone becomes irreversible, and Total Hip Replacement (THR) becomes the only viable option. In this procedure, the damaged hip joint is replaced with an artificial one. THR is a highly effective treatment for relieving pain and restoring function in patients with advanced AVN.
Uncemented vs. Cemented Hip Replacements
There are two primary types of hip replacements: cemented and uncemented. In Uncemented THR, the prosthesis is press-fitted into the bone, which allows natural bone growth to secure the implant over time. This method is often preferred for younger patients as it offers better long-term outcomes. Cemented hip replacements, on the other hand, use bone cement to attach the prosthesis to the bone and are typically used in older patients with Osteoporosis and weaker bones.
For most cases of AVN, uncemented THR is the preferred option, especially for younger patients. The choice of materials for the prosthesis is also important. A ceramic-on-polyethylene surface is often favored due to its durability and lower risk of wear, offering a lifespan of 25 to 30 years in many cases.
Role of Dual Mobility Implants
Dual Mobility Implant Reduces the chances of Dislocation Post Surgery and also helps to Gain more movements. Although it’s not recommended for routine primary cases and reserved for Revision Hip Replacement, cases with higher chances for dislocation. For Primary cases author does not recommend Dual Mobility just to get more movements.
Longevity and Revision Surgery
With advances in surgical techniques and materials, modern hip replacements can last 25 to 30 years. However, in rare cases, a revision surgery may be required if the prosthesis wears out or becomes loose over time. Revision surgery is more complex than the initial replacement but is a possible option for patients who experience complications after their first THR and post-surgery recovery is also good.
Post-COVID AVN of the hip joint is an emerging challenge, particularly affecting young male patients. Early diagnosis and intervention are critical to managing the condition and preserving joint function. While medical management and procedures like core decompression and stem cell therapy can be effective in early stages, Total Hip Replacement remains the best option for advanced AVN. With modern surgical techniques, THR offers a long-lasting solution, improving patients’ quality of life and mobility for decades to come.
For more information and personalized orthopedic treatment in Ahmedabad, consult Dr. Rachit Sheth at Synergy Hospital, Gota.